Investigating New Treatments for Lung Cancer Patients
Credit: National Cancer Institute \ Massey Cancer Center at Virginia Commonwealth University

“You hear the words come out of their mouths, that you have this horrible tumor in the middle of your chest, and you think: cancer means death. I was supposed to be gone 11 months after my initial lung cancer diagnosis. I have beat that by two years so far and I'm not stopping. I qualified for a new clinical trial, Lung-MAP, that was going to be a lifesaver, and it worked for me. I know how blessed I am.”
— Carol "Annie" Burke, Lung-MAP patient
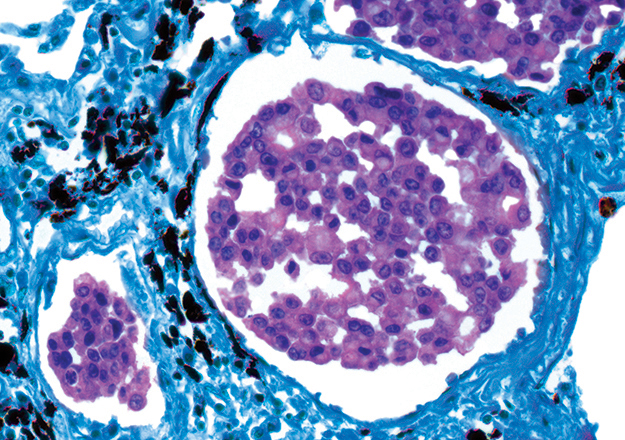
Shortness of breath. Exhaustion. Loss of appetite. These are just some of the symptoms experienced by patients with lung and bronchial cancer, which remains the second most common cancer diagnosis in the United States according to the National Cancer Institute (NCI). About 85 percent of those diagnosed have non-small cell lung cancer, a disease in which cancer cells form in the tissues of the lung.
In 2018, the FNIH, NCI and partners prepared for a major expansion of the Lung Cancer Master Protocol (Lung-MAP) clinical trial. The trial previously tested treatments for people with advanced stage squamous cell lung cancer. It is now open to patients with all types of advanced stage non-small cell lung cancer. This development will enable thousands of new patients to enroll in Lung-MAP, joining the more than 1,800 patients, like Annie Burke, already participating at 640 U.S. medical centers and community hospitals across the country.
Launched in 2014, Lung-MAP is the first major NCI cancer trial to test multiple cancer treatments simultaneously under one "umbrella" design. This pioneering research model is more flexible and faster than traditional clinical trials as it enables researchers to share one trial structure and recruitment process. Patients are tested once for more than 200 cancer-related genetic alterations before they are assigned to investigational treatment studies based on their unique tumor profile. Patients without a matching genetic alteration for a corresponding therapy within Lung-MAP are placed on an immunotherapy regime.
“A great thing about the Lung-MAP design is that the patients can move from one study to the next to the next,” said Jessica Jordan, Research Coordinator, VA Connecticut Healthcare Systems. “Every single study these days requires tissue. We only have to submit one block of tissue and a patient is potentially able to receive more than one line of treatment on the trial if their general health allows. That's the major benefit.”
The trial has already completed seven out of 10 launched studies, with two more sub-studies scheduled to open in 2019, offering patients a personalized approach to finding the investigational drugs that will fight their cancer.
Read more at fnih.org/LungMAP.